Ben Behind His Voices Blog
One Family’s Journey from the Chaos of Schizophrenia to Hope
NEW!– the Ben Behind His Voices audiobook has been updated with a new intro, epilogue, and bonus material! – available only in audiobook form. (updated 2022)
Hear all of the original award-nominated memoir, and find out what has happened in the decade since. We continue our journey through crisis, help, and into hope.
Journalists, Stop Saying “Against Their Will” — It’s About Care, Not Force
No, my son is not okay. He just hasn’t been hurt badly enough yet to qualify for treatment.
What does it take?
In stories about efforts to address homelessness—especially when severe mental illness is involved—the phrase "against their will" is repeated like a drumbeat.
Last month in NYC, a woman was set on fire and burned to death on a subway train in Brooklyn.
The victim, Debrina Kawam, 57, had spent time in a homeless shelter in NYC. Did she have substance abuse issues? According to the New York Times, she did. Mental illness? No official word yet, but it often pairs with substance abuse.
In any event, if she had been placed into treatment, even “against her will,” she would probably be alive today.
Sebastian Zapeta, 33, is accused of starting the blaze with a lighter while Ms Kawam was asleep. He allegedly fanned the flames with a shirt and then watched the fire grow from a bench outside the subway car.
Mr Zapeta claims to have no memory of the incident. He says he had consumed a lot of alcohol. Hmmm.
These and other recent subway crimes have prompted NY Governor Kathy Hochul to announce plans to spend $1 billion to revamp care, and strengthen New York's involuntary commitment laws.
According to CBS News, “she also called for making changes to Kendra's Law, which provides court-ordered outpatient care for people who are at risk to themselves, or others.”
Yes, please.
I have a beef, though: please stop using the phrase “against their will” when talking about getting those with mental illness into treatment.
When people like my son are symptomatic, their “will” is seriously flawed. They’re often psychotic, which means they have a defective or lost contact with reality.
Again, I ask: if someone with Alzheimer’s disease refused help, would you just let them wander around?
The other word I have issue with is “dangerous” when describing those with mental illness. I hear that a lot, and it’s, at best, incomplete.
Why do we so often describe those with psychosis as “dangerously mentally ill”? That was the description I heard on the radio yesterday along with the phrase “against their will.”
Are they dangerous? Yes, sure, sometimes, But. more likely, they are vulnerable -the “vulnerable mentally ill.”
NYC - Above Ground
People like Debrina Kawam. People like my son.
A few weeks ago, I wrote about how my son, Ben, was soon to be homeless. Well, he isn’t, yet, because he refuses to move out of his affordable housing.But he will soon be evicted, unless we can get him to “come to his senses” and find another place to live.
Come to his senses? Ha! That is precisely the problem.
Ben is refusing treatment, He is often high, or worse. He has stopped his meds. And, because of that, he has become a victim. He is committing no harm to others, but has been forced from his apartment by dealers who have taken it over and “allow” him to sleep on his own couch, probably in exchange for drugs.
My son no longer asks me for money. He doesn't ask for help. He doesn’t ask for anything.
He just spends all day at a clubhouse for the homeless, eating free meals, listening to loud music on his headphones, keeping to himself. Then I guess he goes home to sleep on his couch…while he still has one.
“Dangerous? Sometimes, But. more likely, they are vulnerable -the ‘vulnerable mentally ill.’”
This is a person who, five short years ago, was a full-time restaurant server with 5-star reviews, driving a Lexus, paying taxes. Then Covid came, marijuana followed, and he broke down.
Is he okay? No!
Does he think he is okay?
Sadly, yes.
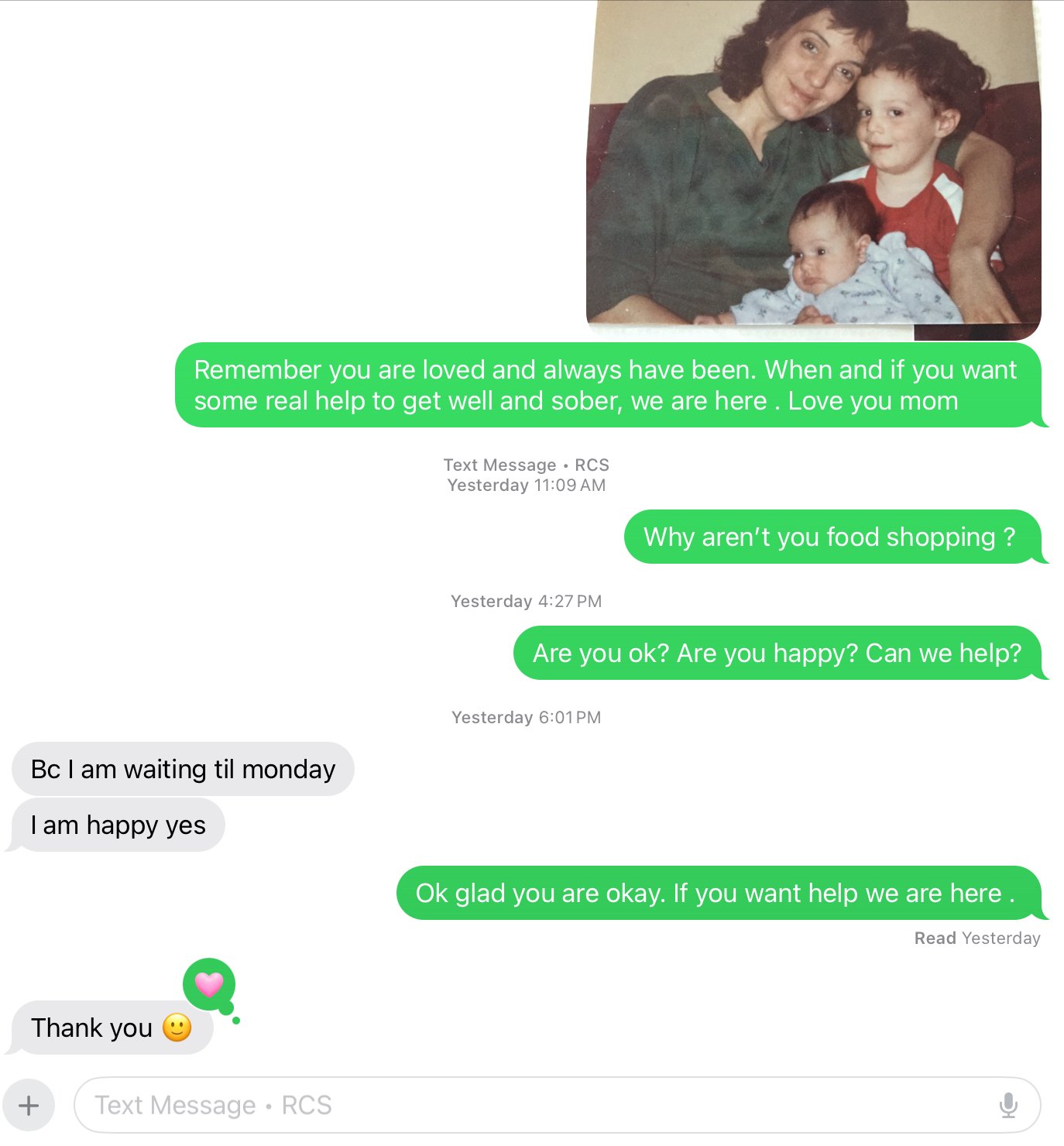
See this text exchange from yesterday:
text exchange of love, hope and lack of insight
No, my son is not okay. He just hasn’t been hurt badly enough yet to qualify for treatment.
What does it take?
In stories about efforts to address homelessness—especially when severe mental illness is involved—the phrase "against their will" is repeated like a drumbeat. It’s a phrase that carries weight, evoking images of force, violation, and a stripping away of autonomy. But it's also a phrase that simplifies, distorts, and ultimately misrepresents the reality for so many vulnerable people.
When someone is experiencing a severe mental health crisis—living unsheltered, disconnected from reality, and unable to meet their most basic needs—their will isn't always clear, consistent, or capable of prioritizing their own safety. Mental illness can cloud judgment, distort perceptions, and create deep mistrust, even toward those trying to help - like their case managers, or their family.
Journalists, with their power to shape public opinion, need to be careful with the words they choose.
"Against their will" suggests a struggle between personal freedom and intervention. But what if we reframed this? What if we recognized that leaving someone to suffer on the streets, untreated and exposed, isn't an exercise of freedom—it's neglect.
“No, my son is not okay. He just hasn’t been hurt badly enough yet to qualify for treatment.”
And it’s not just about danger. Too often, media narratives focus on whether someone poses a risk to others. But vulnerability is its own emergency. A person shivering on a sidewalk in winter, malnourished, delusional, and isolated, doesn’t need to be dangerous to deserve care—they need to be human. They are vulnerable.
My son is one of these people. Today, he tells me he's fine, happy, and doesn't need help. But five years ago, while in treatment, he was gainfully employed, contributing to society, and connected to his family. He was genuinely happier. Now, he believes he’s okay, but he’s not. His reality is distorted by an illness he cannot see, and his refusal of care isn’t a sign of independence—it’s a symptom of his condition.
This isn’t about stripping away rights. It’s about recognizing that dignity includes access to shelter, treatment, and a chance at stability. It’s about understanding that severe mental illness can impair someone's ability to make informed decisions about their own care. It’s about seeing intervention not as coercion, but as compassion.
About a year ago, we interviewed Brian Stettin, senior advisor on severe mental illness to NYC Mayor Eric Adams, on our podcast, Schizophrenia: 3 Moms in the Trenches. We will do a follow-up interview this month, but at that time Brian was talking about how enforcing Kendra’s Law has helped people reconnect with their families, get off the streets, find life again. All, initially “against their will.”
So, to journalists: Please reconsider the phrase "against their will." Instead, talk about support, care, and connection. Focus on the vulnerability that makes intervention necessary, not just the potential for harm.
Words matter. And in this case, they could make the difference between reinforcing stigma and building understanding.
Happy Despite Love?: Holiday Season in the Time of Schizophrenia
Yes, I always dare to hope. Maybe, just maybe, he will come back to us again. And then, maybe, we will lose him again.
Until then, we fight.
I haven't seen my son Ben in almost two months. The only time I hear from him is if he needs something from CVS. Then I buy it online, leave it at his local store for pick-up, and hope he won’t trade shampoo and conditioner for drugs. (Is that even a thing?)
Other than last year, when Ben was in jail pre-trial, this is the first set of December Holidays without my son.
Thanks for your comments, shares, and subscriptions to my last post, sharing the family experience as our loved ones spiral downwards. Though I write about many aspects of life’s imperfections, posts about my son’s mental illness oftem seem to strike the loudest chord.
For us, and maybe for you, The Holidays are particularly hard. This Hallmark benchmark of family reunions, end-of-year forgiveness, and new beginnings elude those of us who have a loved one out there in the streets, refusing help or treatment.
So - can we be happy anyway? How can we celebrate?
Because we must.
Because, even though we love (and grieve) our missing loved ones with all our hearts, life has to be more than the fierce despair, hope, and determination that all families feel when a mentally ill loved one is lost to us, yet still here.
Danger - yet the door is open
It’s the “ambiguous loss” of no closure, of a door marked “DANGER” that is always ajar - or, sometimes, wide open.
In the novel Love in the Time of Cholera, (full disclosure, I have yet to read it - but a character in another novel I loved -The Bird Hotel - shared this quote):
"One could be happy not only without love, but despite it.".
This line (attributed to Fermina Daza, who experiences a complicated relationship) highlights the complex nature of love in the novel, suggesting that true happiness can sometimes exist even when love is not present or is unfulfilled.
Boy oh boy, if ever there were a “complicated relationship”, loving someone with an SMI (Severe Mental Illness) is a textbook example.
For me, the part of the quote tha rings most true is about being happy despite love. For, of course, I love my son with all my heart. My daughter loves her brother, her kids love their uncle.
…a different kind of Holiday season
And yet this love is underneath the loss and sadness we feel, especially around the holidays.
Can we be “happy” anyway?
Well, yes. At least some, or maybe most, of the time.
There is a saying I often hear quoted: “You’re only as happy as your unhappiest child.”
I have had to choose to throw that belief away. To choose to let anyone else choose my emotions for me - even my first-born child - would be a disservice to the rest of my life: to family, to friends, to work, to art, to nature, to reality.
I choose happier. This isn’t always easy. But I choose it.
And, of course, cry when I need to.
But here’s the hardest question: Does Ben’s life have “worth” right now?
Would I have chosen to give birth to him, knowing the heartaches ahead for us all?
Yes I know. No one wants to ask that question.
Yet those of us who have mentally ill loved ones do ask it at times. We do. For it hurts so much to see them suffer, and to be powerless to help - emotionally, financially, and legally.
Ben won’t/can’t accept our love right now.
He will do anything for his next fix.
His teeth are so unhealthy they could become infected and cause his death.
He is about to be evicted - or arrested.
His so-called “friends” are actually drug dealers taking advantage of him.
Families ask: What kind of a life is that?
Me? I am compartmentalizing like crazy.
I do my work.
I help and celebrate with my family (what’s left of it).
I go to storytelling class.
I go to parties, to the movies, out to dinner..
I binge-watch Only Murders in the Building with my husband.
I live my life.
I do my podcast.
He made me a Mom, my daughter a sister.
I go to AlAnon.
Because that is how I can cope.
Happy despite love, despite the missing piece in my life.
I’m not without my son’s love right now, looking at the big picture. He’s still the same being who made me a mom, who taught me about unconditional love just by existing, who challenged me, made me laugh, made me angry and frustrated, made me so proud.
I love my son.
I can pretend he is away in a different way, in the ways he used to be - doing volunteer work, at summer camp, on a teen trip, in a program.
I can be grateful to the few people who are also doing their best to keep him safe (an attorney, some case managers, a nursing agency, the police).
I can focus on what is still so good in my life and help nurse the many broken hearts caused by my son’s dual illnesses (schizophrenia, and now addiction).
Yes, I will be happy despite love. Most of the time.
Like all families I know, of course I will do my best to help when help is asked for - and sometimes when it isn’t.
But, in the meantime, I remind myself about all the joy that loving Ben has brought to all our lives.
This is the person who made me a mother. Made my daughter a sister. Taught my husband about step parenting. We would not be the same without loving Ben.
Yes, I always dare to hope. Maybe, just maybe, he will come back to us again. And then, maybe, we will lose him again.
Until then, we fight.
We fight to make the system better.
We fight to raise awareness.
We fight for more research.
We fight for treatment before tragedy.
We fight to stay happy.
We fight for love, for justice, for a miracle. ‘Tis the season.
Happy Holidays, however you celebrate.
Luigi Mangione, Jordan Neely: Mental Illness in the News? One Mother’s Opinion
Where has the family been, where SMI is concerned?
We’ve been right here all along. Help us help. And - unless you have been in our shoes - stop with the comments and the snap judgments. Ask us questions instead. We are living in the trenches.
About a month ago I wrote about how my son, Ben, was close to homelessness. At the moment he is still housed, but facing eviction. Why? Because he repeatedly breaks the rules in the lease, endangering others in the building with his addict lifestyle. That is a consequence of his own choices, illogical as they may be. He needs treatment, and no one is allowed to step in to “require” it.
No. He is not “sick enough.” Running alongside my car last month, trying to jump into the driver’s seat to stop my car so he could have extra money? Not an “imminent danger” to himself or others.
Huh??
I beg to differ.
But there is no mandate requiring Ben to have the treatment he needs. My hands are tied, and I can only “help” from afar while trying to protect others that I love.
Lately, two events have brought the question of untreated mental illness to the forefront: the stories of Jordan Neely, who died by vigilante chokehold when he was frightening subway passengers, and Luigi Mangione, who murdered a Healthcare CEO in premeditated cold blood and is still somehow being hailed by some as a hero.
No. Not a Hero. But possibly very ill, with a family helpless to help.
Jordan Neely was diagnosed with schizophrenia, exacerbated by the tragic murder of his mother. He was homeless at the time of his death.
My son’s behavior when trying to get money for a fix (though of course he said it was for a concert) frightened his family enough for me to get a protective order in place. For now we send his money for rent and food, but cannot (and should not) let the behavior that is leading to his eviction be excused.
That’s us. As for Neely, I don’t know what went down in that subway car. I wasn’t there, but I do know this: the only thing worse than my son hurting himself would be if he were responsible for hurting another human being. That guilt…I can only imagine. I never want to know.
Had Luigi Mangione developed a mental illness in the months before his alleged act? As psychiatrist Dr David Laing Dawson points out, no one is really talking about that right now. But signs are there, as are stories of how hard his family searched for him when he went missing.
One thing is consistent, though, in comments on social media. People keep saying, “how could they have gotten this far? Where was the family?”
When Treatment Works, The Love is Returned.
I’ll tell you where the family has been. At least this family.
This family, like so many others, has been working for years to “save” our loved one with SMI (severe mental illness) and blocked at every turn by:
anosognosia (their lack of awareness that they are ill),
substance use and abuse (often a self-medicating beginning to addiction when SMI is present)
Lack of psychiatric hospital beds
Lack of funding for more research
Blame for families
Stigma against SMI,and
a system that puts “patient rights” to homelessness, hunger, crime, addiction, and other “freedoms” about the right to be safe and get treatment.
“This family, like so many others, has been working for years to “save” our loved one with SMI (severe mental illness) and blocked at every turn.”
So - where have we been, as my son Ben faces addiction and homelessness?
Right where we have been for the past two decades, ever since his diagnosis of schizophrenia:
Trying to help
Trying to arrange help
Fixing what we can.
Letting natural consequences settle - usually to no avail.
Setting boundaries.
Leaving the door open - or closing it tight if we are afraid for our safety.
Searching the streets.
Advocating for change.
Reaching out to each other.
Reversing their bad decisions.
Keeping young children away when our loved one is symptomatic,
Talking to attorneys.
Paying for rehab and “troubled teen” programs.
Declaring bankruptcy.
Visiting hospitals and jails.
Educating ourselves.
Daring to hope.
Fighting with all our heart.
We’ve been right here all along. Help us help. And - unless you have been in our shoes - stop with the comments and the snap judgments. Ask us questions instead. We are living in the trenches.
My Son Will Be Homeless This Friday. Here's Why It Didn't Need to Happen.
This Friday my own son will be out there, unhoused, too. Not by the grace of God, but by the grace of addiction, schizophrenia, a system that protects his “rights” to live unhoused over getting treatment, and by a mother who, this time, will not rescue him.
Two weeks ago, I was walking through Chicago streets during breaks in the Voiceover Conference I was attending. The weather was beautiful, the Public Transportation efficient and smooth, the city a delight.
And still…there were unhoused humans everywhere - on a park bench, napping on the floor of the train stations, outside the restaurants and CVS.
Unhoused, filthy, muttering to themselves.
And I thought, my son is a heartbeat away from this. I have saved him from this more times than I can count. He is among the lucky. There but for the grace of God…
But this Friday my own son will be out there too. Not by the grace of God, but by the grace of addiction, schizophrenia, a system that protects his “rights” to live unhoused over getting treatment, and by a mother who, this time, will not rescue him.
He has to hit bottom. Real bottom. But, sadly, he has been there before.
His SMI (serious mental illness), when untreated, interferes with his ability to know he has hit bottom. The voices which he swears he does not hear will tell him it’s okay. That he is okay. That his mother, sister, and whale family are crazy, not him. That he doesn’t need help. This is just fine.
Yes, the PC Word now is UnHoused. Whatever you name it, in four days my son will be without a place to live, without a bed to sleep in.
And this is my only option, after schizophrenia and addiction took over.
Six short weeks ago, Ben was let loose from jail diversion. The judicial system took away all requirements for his release. No checking in. No drug testing. No structure imposed. All the things that had gotten Ben to the point of recovery up til then: structure, purpose, community. All now -optional. And unchosen.
One directive: “just don’t get into trouble”.
And for two golden days, it all looked hopeful. He connected with old friends, said he had learned his lesson, hugged his nieces and nephew, admitted for the first time that he “might” actually have schizophrenia.
All it took was one hit of marijuana, one beer - and his chemical balance was all off. A complete 180 from his recovery mindset.
Marijuana may be legal now - but, for some brains, it is lethal.
Ben is now only six weeks into his freedom - services available but optional - and he has become so unmanageable that the only choice left is to remove him from his housing - before there is an eviction on his record. This is the one and only action I can take to still help preserve what is left of his reputation.
“Marijuana may be legal now - but, for some brains, it is lethal.”
So I will.
I rented the storage unit, I’ve paid the movers, and in four days all my son’s brand-new furniture and household goods (we were so hopeful when we bought them) will be moved to storage. I will tell my only son to pack a bag and wish him luck.
I will speed him to homelessness.
Maybe the people who have been crashing in his bedroom (leaving him to sleep on the loveseat) will have a couch he can crash on.
Maybe he will stop using, now that he has no housing to trade for drugs.
Maybe - just maybe - he will take his agency up on the only other offered option: check yourself into the hospital and ask for detox and rehab.
At least he will have a bed there.
What could have prevented this?
Assisted Outpatient Treatment. Connecticut is one of only two states to not have this in place.
According to the Treatment Advocacy Center, “Assisted outpatient treatment (AOT) is the practice of providing outpatient treatment under civil court order to individuals with severe mental illness (SMI) who have demonstrated difficulty engaging with treatment on a voluntary basis. When systematically implemented and adequately resourced, AOT can dramatically reduce hospitalization, criminalization, and other adverse outcomes for its target population”
If Ben had been court-ordered into treatment, he might be on his way back to employment, community, and sobriety.
But every single time we have called for him to be evaluated (by police or mental health teams), we’ve been told,
“we can’t help him without his consent.”
“He isn’t a harm to himself or others yet”
”He isn’t sick enough.”
I have heard all this before. And, again, I beg to differ.
You may ask, Why don’t I take him back home?
Because I am now frightened of my own son. Not my sober son, but my addicted son. I have seen what drug use makes him do, how he justifies theft and fraud and family pain.
So my only choice is to let him hit bottom.
The fact that in order to do that, I must supervise the removal of all his possessions from his apartment to a storage unit, watch the movers take it all away while Ben protests, breaks my heart.
But I have no choice left.
It must be done.
Ben has had help offered to him, but is in no place to really accept it. Social workers everywhere, I salute you. But as the agency trying to help my son says they say to their staff, “We can’t be working harder than the client.”
I know.
My son must want to be helped.
He does not. His illness and addiction won’t let him think that.
So down down down he will go.
I just hope he knows he has hit bottom when he gets there. And that he remembers all the love he has had in his life. I hope it can,eventually, come back to him.
How I miss who he used to be, even six weeks ago.
This did not have to happen. But is it happening.
This Is Who the Universe Gave Me to Take Care of…and I Need Help
I’m scared of - and scared for - this beautiful person I gave birth to 42 years ago.
Universe, I quit this job. I’m done. How I wish I could. I’ve supported him through more crises related to his mental illness than I can count - picked up the sharp pieces and helped him rebuild.
But I cannot “support” him through addiction…and my own destruction
I have fought my son's schizophrenia for over 25 years, ever since his diagnosis, and for years before that, as the symptoms appeared and escalated.
Mom it is after 12 can hv today's money?
A text from the person who has been told - by the police - that he is not to contact me before his court date, which is today. Because I am the “victim” in this case.
It says so on the police report I filled out last night.
The victim of my son’s abuse - verbal but relentless, And I no longer believe it could never escalate beyond this.
I’m scared of - and scared for - this beautiful person I gave birth to 42 years ago.
Universe, I quit this job. I’m done. How I wish I could. I’ve supported him through more crises related to his mental illness than I can count - picked up the sharp pieces and helped him rebuild.
But I cannot “support” him through addiction…and my own destruction
I have fought my son's schizophrenia for over 25 years, ever since his diagnosis, and for years before that, as the symptoms appeared and escalated.
“I’m scared of - and scared for - this beautiful person I gave birth to 42 years ago.”
Believe me, I have done my best. My absolute best.
Let me count the ways:
Troubled teen residential programs in Montana and Idaho.
Three apartments rented, furnished, supported…and dismantled.
Three group homes.
Nine years of medication supervision and free rent in my home,
Ten hospitalizations.
Help getting him out of two arrests - the second time to get him into a jail diversion program.
Serving as conservator of estate and person - fixing financial disasters, helping practitioners help him with careful record-keeping and consultation.
I knew my son’s behavior wasn’t his fault - it’s an illness with the added bonus of anosognosia (he doesn’t know he is ill)
I learned about schizophrenia, wrote a book about it, host a podcast about it, helped other families cope as a NAMI Family-to-Family teacher and trainer.
I’ve been turning the pain into purpose for decades, steadfastly collecting the memories of good days when my son was “almost normal”, making peace with this by telling myself that this is who the Universe gave me to take care of.
I was up to the job.
But I can’t do it anymore - not now that substance abuse has entered the picture.
For over two hours yesterday I retreated from my son as he followed me around a shopping center and then his neighborhood, screaming that I had to give him the money I had set aside to pay for the dental work he has to have. This is why he has a conservator - to make the decisions he is not capable of making.
While he had been in jail this year awaiting a bed in the diversion program, some money had accumulated for him - enough to set him up in a fresh start. We celebrated his “graduation” with some new furniture, some clothes, and kept some aside for the college classes he wanted to take, the used car he hoped to buy, and to pay an oral surgeon to pull the rotted teeth that were causing so much pain, preventing him from landing jobs, and were threatening his life.
He was so excited.
For two days.
And then, I suspect, he started using substances again. Marijuana for sure, but it has to be more than that. The change in him is extreme.
My son currently looks alder than I do. No life in his face. Bags under his eyes. Dirty fingernails. Muscle twitches in his hands and jaw. Is that Haldol side effects? - or is his street purchase of marijuana laced with fentanyl?
We had set a budget together, but he kept asking for the money we’d set aside as well. He wore me down asking and asking and asking. Part of me was glad he wouldn’t have enough for a car, because I could see he was in no condition to drive anymore. Before I knew it, all that was left was the money for the dental work, and I stopped giving in.
Like a toddler who doesn’t get the toy he wants, my son escalated his begging, yelling, and tantruming for over two hours. Every time I got in my car to get away from him, he popped into the passenger seat before I could lock him out. Every time I exited the car, he got out and followed me everywhere, as I retreated down the block and into alleys and driveways.
This is what the passers-by saw: me, walking away, attempting to calm myself with mantras like “it’s his illness, it’s not him”.
Him, two steps, behind, saying the same things over and over:
“It’s my money, it’s not your money”
“Just listen to me.”
“You can’t make decisions for me. It’s my money.”
“I want to go clubbing tonight.”
“You can’t tell me what to do.”
“Give me my money!!!!”
“Are you too stupid to understand?”
This is not schizophrenia. This is drug-induced mania. I don’t know what he is using, but I’ve never seen marijuana do this.
Back to my vehicle. After a few tries, I finally succeed in locking my son out of the car.
He stands in front of it, blocking my way.
When he gets distracted enough to move away I take off down the driveway of his supported housing building - and he runs alongside, pulling open the driver’s side door and trying to get in to stop me.
I keep driving. This is my only chance to escape.
He is knocked to the ground, but okay enough to get back up and run after the car.
This man, the boy I raised, this child whose first act after graduating from jail diversion was to buy gifts for his nieces and nephew because he had missed their birthdays, is the source of my terror now.
So I call the police. Ask for a mental health crisis team for him.
But he had already called them to accuse me of abuse.
I drive back to his apartment complex. Wait in my locked car for the officers to arrive, hoping I don’t see my son try to get into my car again.
I think about what I’ll say to my husband if they arrest me.
Eventually after taking our statements, the police charge my son with breach of peace and interfering with a 911 call (he had ripped the phone out of my hands when I had said I was calling the police, that he was scaring me).
I ask for him to be sent to the hospital for a 72-hour hold, but hear the all-too-familiar, “sorry, he’s not sick enough.”
Not a harm to himself or others. Really? After trying to carjack his mother, being knocked down in the process?
So they arrest him, take him to the station to be fingerprinted and processed - and later he s released on promise to appear in court today, with clear instructions not to contact the victim - me.
It’s 2 am now. I couldn’t sleep for more than three hours.
And wake up to that text, sent immediately after midnight. Delete it after the screenshot. Even directives from the police couldn’t stop him from asking for cash.
I have no more fight in me, with two enemies now: schizophrenia and now substance abuse.
Tomorrow, I find an attorney to be the conservator. I can’t do that job anymore. I’ll always be his mother, but I can’t save him again.
Universe, I’ve done my best. I have other people to take care of. As they remind me at AlAnon,
It’s his journey too.
Between Psychosis and Success: What if Your “PosSCZible” is Somewhere in the Middle?
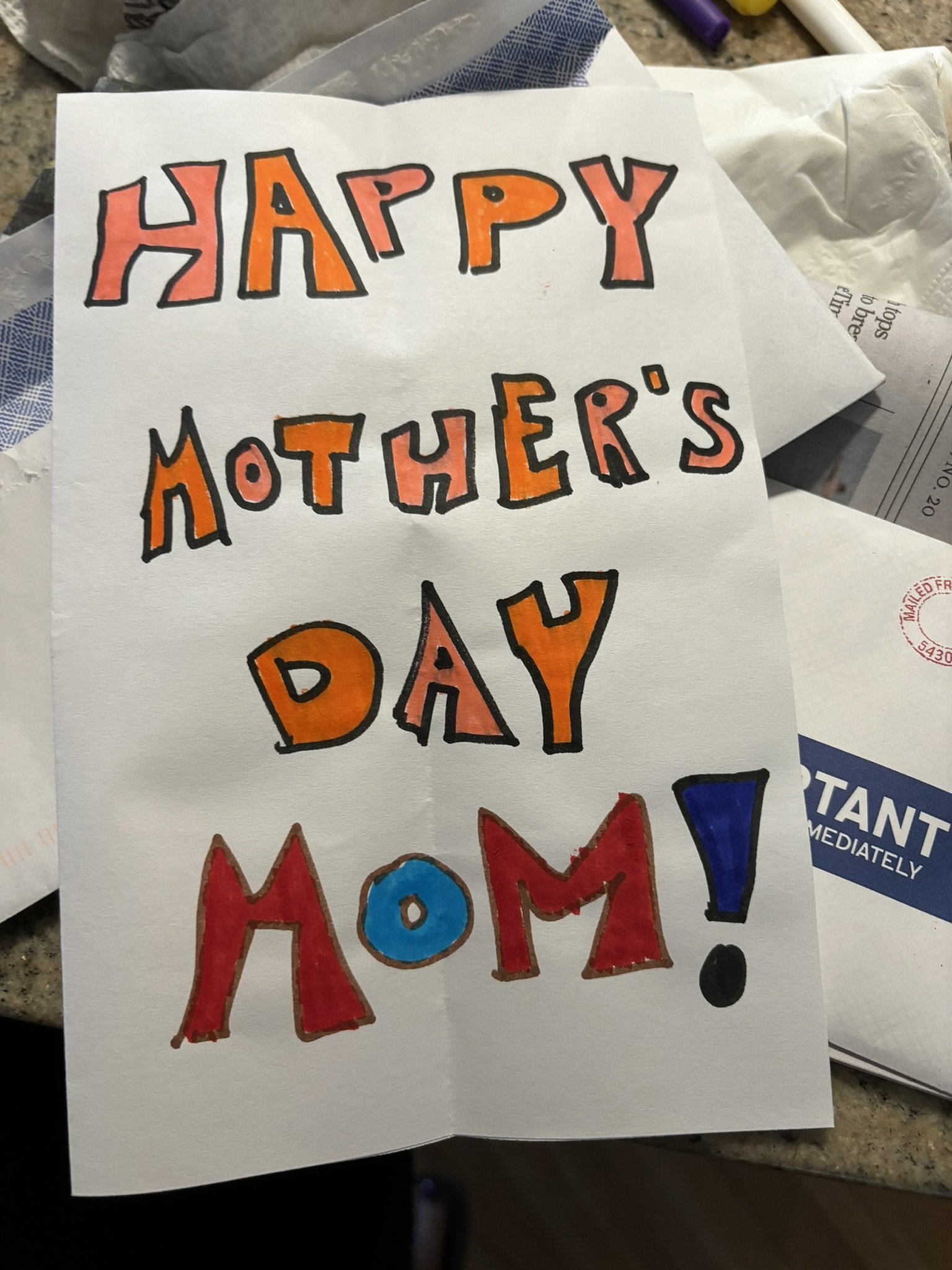
For some, just staying out of the hospital is a victory. Staying away from substances that take the pain away, temporarily, is a victory. Getting a birthday present. Going to Thanksgiving Dinner.
Or, in our case, sending your Mom a Mother’s Day Card.
May 24 is World Schizophrenia Awareness Day, and Bristol Myers Squibb has launched a new campaign, Live Your PosSCZible" with today’s news featuring Taye Diggs interviewing his lovely sister Christian, currently in recovery from schizophrenia and living her “Possczible.”
I’m thrilled that this illness is getting some attention, probably new treatment, and - most of all - hope. Not to mention a call to reduce stigma, and spotlight the human face of SZ, and what is possible.
I am all for it.
In fact, we have interviewed many of the people featured in this campaign on our podcast, Schizophrenia: 3 Moms in the Trenches. Impressive indeed. And kudos to all. Seriously. I mean that with all my heart.
But (to channel Carrie Bradshaw) I couldn’t help but wonder:
What about all the people like my son, whose picture of “recovery” is quite different? Who is far from a poster child for recovery from schizophrenia? Whose “good years” - in treatment and with gainful employment - still looked, to many, like something was not quite right?
I used to say, during those years (when Ben was taking his medication regularly - only because it was a house rule, but hey) “I’ve got my son back, to an extent. Let’s say, 65%. But I’ll take it!”
I knew, and I still know, that 65% back is a miracle.
But my son is not represented in this campaign. He would never agree to it. Why? Because he doesn’t believe he has schizophrenia - and that, my friends, is the big obstacle.
You see, all the success stories presented in this campaign - and also on many episodes of our own podcast - have this in common: they know they have schizophrenia.
They do not have anosognosia. (the lack of awareness that you are ill)
Maybe they once did, but they don’t now. They take their medication, they accept treatment.
But what about my son, and thousands like him?
Why are the stories of the “in-betweens” not covered in these campaigns?
People who, like my son, did not get diagnosed early enough to ward off brain damage? Those who developed first symptoms in their mid-teens, not (as is more common with women) in their 20’s?
What does “Possczible” look like for them?
Ben is finally - finally - out of jail where he was held, pretrial, for nine months, waiting for a bed in a diversion program. His teeth are black from his meds. He barely makes enough to afford housing when he graduates.
Holding a job is hard, as his symptoms can return when it comes closer to the time he has his monthly long-acting injection. He could supplement with a daily med, but he doesn’t think he has an illness. He only takes the meds because he has to - for this program, for his family.
Still he has this in common with Taye Diggs’ sister (and many others in the “success story” categories) - family support. He has his family’s love - and often their help.
Not everyone in recovery from this devastating illness has a Masters’ Degree and a Full-Time job. For some, just staying out of the hospital is a victory. Staying away from substances that take the pain away, temporarily, is a victory. Getting a birthday present. Going to Thanksgiving Dinner.
Or, in our case, sending your Mom a Mother’s Day Card.
Bristol Myers Squibb and all of you - thanks for this campaign. Anything is better than stigma. But let’s not leave out the people in the middle - and their families and caregivers.
We need Possible too.
Mental Health Awareness Month: Guest Blogger, Beth Lazar
In honor of Mental Health Awareness Month, a member of my faith community, a Reform Jewish Congregation, presented this sermon.
Beth co-chairs the Mental Health Awareness Team , and concludes:
“Our forefathers in Biblical times excluded the disabled from the Temple ritual of burnt sacrifices. Today, modern Reform Jews include, accommodate, and try to better the lives of people with disabilities, including people with mental illness. I feel comfortable and supported at B’nai Israel, and I’m glad I’m a member.
In honor of Mental Health Awareness Month, a member of my faith community, a Reform Jewish Congregation, presented this sermon.
Beth co-chairs the Mental Health Awareness Team , and concludes:
“Our forefathers in Biblical times excluded the disabled from the Temple ritual of burnt sacrifices.Today, modern Reform Jews include, accommodate, and try to better the lives of people with disabilities, including people with mental illness. I feel comfortable and supported at B’nai Israel, and I’m glad I’m a member. Shabbat Shalom.”
Sermon about Mental Illness by Beth Lazar
Torah Portion: Emor, Leviticus 21, lines 18-21
May is Mental Health Awareness Month. Mental illness is often referred to as a disability. What does the Torah say about people with disabilities?
This week’s Torah portion, Emor, Leviticus 21, says this about those who can make an animal burnt sacrifice, which is how our ancestors communed with God:
No man who has a defect shall be qualified to offer the food of his God. No one at all who has a defect shall be qualified. No man who is blind or lame or has a limb too short or too long. No man who has a broken leg or broken arm or who is hunchback or dwarf, has a growth in his eye, who has a boil, a scar, scurvy, or crushed testes.
Unlike our ancestors who excluded the disabled, modern Reform synagogues try to include the physically disabled by providing ramps and elevators and amplification for the hearing-impaired, and now zoom helps too.
In 2001, the Union for Reform Judaism, the URJ, adopted 13 resolutions regarding mental illness. Resolution #2A calls on congregations to participate in communal efforts aimed at destigmatizing mental illness. This sermon is a step in fulfilling the goal of this resolution.
The words “mental” and “mentally ill” are often used as pejoratives to describe someone you disagree with or think is evil or violent, such as political opponents, Nazis, racists, and people who commit mass shootings. In fact, mentally ill people come in all different political persuasions, nationalities, races, and genders. Mental illness is not the cause of mass shootings and violence. To the contrary, mentally ill people are 4 times more likely to be victims of violent crime compared to the general public. Mental illness is all over the world, yet only in the United States are there so many mass shootings and daily deaths by gun violence. This is due to the proliferation and easy access to all guns including military-style guns.
In truth, there is nothing shameful or evil about being mentally ill. Mental illness is an illness of the brain. Depression and schizophrenia are caused by the body’s deficiency in the production of certain brain chemicals needed for the functioning of a healthy mind. Just like the chronic illness of diabetes, where the body doesn’t produce enough insulin. Mental illness is an illness, not a character flaw.
As artist Vincent Van Gogh, who struggled with schizophrenia, wrote to his brother back in 1889,
As for me, you must know, I shouldn’t precisely have chosen madness if there had been any choice. What consoles me is that I am beginning to consider madness as an illness like any other and that I accept it as such.
Other famous people struggled with mental illness. Writer Sylvia Plath had depression. Actor and stand-up comic Robin Williams had bipolar disorder. Nobel Peace Prize winner in economics John Nash had schizophrenia. Some people romanticize mental illness as an enhancer of genius and creativity: the mad scientist, the crazy creative artist. In reality, mental illness does NOT enhance creativity but instead is a big stumbling block. For example, John Nash had his career interrupted by having a major psychotic episode. He spent time in a mental hospital before he could resume his work.
I can testify that mental illness interrupted my schooling and creativity. In 1984, I had completed all my master’s course work and had planned to write my master’s thesis and earn my master’s degree by the end of 1985. My plan was interrupted by mental illness and multiple hospitalizations. I didn’t earn my master’s degree until 1989.
Vincent Van Gogh, Sylvia Plath, and Robin Williams all died by suicide caused by mental illness. Mental illness is the death of creativity in cases such as suicide.
Depression is the leading cause of suicide. Each year, 40,000 people die by suicide in the USA. That’s the same number of people who died from breast cancer. The issue of suicide should have the same amount of public attention, support, treatment, funding and medical research as the issue of breast cancer does.
Anyone concerned about people with mental illness should be concerned about the criminal legal system and mass incarceration because there are 10 times more mentally ill people in jails and prisons than in mental hospitals. According to the Bureau of Justice statistics, 44% of people in jails and 35% of those in state and federal prisons have a mental illness. 3 out of every 4 children in juvenile detention have a mental illness.
There are so many mentally ill people in prison because in the 1980s and 1990s, many state mental hospitals closed. Regular hospitals have a shortage of beds available for psychiatric patients. When mentally ill people don’t get the treatment they need, they can’t function well, lose their jobs and then their apartments because they don’t have the money for rent.
Once homeless and living on the streets, they get sucked into the criminal legal system. Drugs and alcohol used as a means of self-medication become abused, which together with loitering, disturbing the peace, and petty theft, are reasons the homeless mentally ill are arrested. Lacking money for a good attorney and bail, the mentally ill languish in jails and prisons.
Once in prison, the majority of mentally ill people do NOT receive the mental health treatment they need. Instead, 4 thousand people with serious illness are held in solitary confinement in prisons. Before 2022, Connecticut incarcerated people were subject to months, even years, in solitary confinement.
The organization Stop Solitary CT wrote and lobbied for the Protect Act, a law which restricts the use of solitary confinement to 15 consecutive days in a 60-day period. The law also establishes an independent advisory board to hire an ombudsperson to monitor the CT Department of Corrections. One member of the advisory board must be a mental health care professional. The Protect Act was signed into law May 2022.
URJ resolution #10A states, “Place nonviolent mentally ill offenders into community-based mental health programs. Work to ensure that persons with mental illness who are sentenced to prison receive appropriate and humane treatment, including access to appropriate medication.”
URJ resolution #2B urges synagogues to “Work with persons with mental illness and their families so that they feel welcome within our synagogues.”
B’nai Israel does this, giving members platforms to share their mental health journeys. Congregant Randye Kaye, who is an actress and radio host, presented her book, “Ben Behind His Voices.” It’s the story of how she dealt with having a son who has schizophrenia.
Congregant Ivan Maisel, who is a sportswriter, shared his book, “I Keep Trying to Catch His Eye: A Memoir of Loss, Grief, and Love.” It’s about how he and his family dealt with the death by suicide of his son.
Congregants who are mental health professionals have used their knowledge to serve the congregation. Jennifer Doran did trauma counseling after October 7.
Rachel Yarden leads a support group for caregivers.
Dr. Kerner gave presentations about depression.
Our Rabbis are very supportive of B’nai Israel’s Mental Health Awareness Team, which was founded by me and Adam Weisblatt, and now Marje Freeman and I are co-chairs.
In summary, our forefathers in Biblical times excluded the disabled from the Temple ritual of burnt sacrifices. Today, modern Reform Jews include, accommodate, and try to better the lives of people with disabilities, including people with mental illness. I feel comfortable and supported at B’nai Israel, and I’m glad I’m a member. Shabbat Shalom.
My Son is Anakin too: Schizophrenia Destroys Dreams
Jake Lloyd - known for his childhood role as Anakin Skywalker - has schizophrenia. His mom, Lisa, bravely shares their story. Our son, too, was full of dreams and hopes. Schizophrenia steals. The Lloyd family is not alone.
“Oh, hi Ms. Kaye. You can go on in.”
They recognize me now. I am here so often.
No, I’m not at the Doctor’s office. I’m not on a third job interview.
This voice comes to me through the one-way glass. I can't see the face of the person who is welcoming me.
I'm checking in, once again, to visit my son in jail.
This is my Saturday routine right now: A visit, when no lock-down is in place, and then (a new addition) an Al-Anon meeting to remind myself that this incarceration, and the addiction partially responsible for it, are not in my control.
A reminder to love, and to detach.
Detachment: an ongoing journey ever since schizophrenia stole my son away from us - and away from himself.
If you’ve read my book Ben Behind His Voices, or listened to the podcast I co-created with two other Moms, Schizophrenia: 3 Moms in the Trenches, you may know our family story. If you have had this happen to you, you know it all too well.
One way we cope is to turn agony into advocacy. Hence our books, our podcast, our speaking out in public. In the words of Willie Loman in Death of a Salesman, “Attention must be paid.”
And then I see this in my newsfeed: another Mom in the Trenches.
Her name is Lisa Lloyd, and her son could be my son. The promising early start, the dreams of a successful future and happy life, the confusing changes in high school, the psychosis, the crises, the treatment, the relapses…this story is my story.
Except that Lisa’s son, Jake Lloyd, is famous. Or he was, before the illness. Jake Lloyd played young Anakin Skywalker in Star Wars, and many other roles.
A child star. So, sure, this gets more media attention.
My son, too, was a star - but locally, in our circles, in his school, among his friends, to his family.
I don’t post adult pictures of my son, who has asked to be called “Ben” when I speak about him (not his real name) - but I can post the child pictures of my beautiful boy so the world can see what could have been, and what what once was - and, maybe, what could be again, with help.
I get it: the world is much more interested in celebrity stories, whether it’s about losing five pounds, breaking up a romance, or getting hit with an illness.
Lisa Lloyd could have hidden the truth. Her son, Jake, could have asked her to. But instead they are speaking out, drawing some attention to this devastating illness that steals reality - taking with it dreams, love, and life itself.
So, thank you to Lisa Lloyd. Thank you for your advocacy, for speaking out.
And, if I could meet with you over a cup of coffee, I’d remind you: You are NOT alone. There are countless kindred spirits fighting for respect, treatment, empathy, and - so importantly - a cure.
As of today, my son still waits for a bed to open up in the treatment program he needs, and has qualified for. Like so many, his mental illness (and the accompanying substance use for comfort) has landed him in pretrial jail. The only problem is that there is no room in the program he has been accepted to.
So he - and we - wait. We wait in hope, we wait in frustration, we wait for attention to be paid to this serious mental illness that destroys lives and families.
Lisa Lloyd, we hear you. You are not alone. We wish the best kind of success for Jake, and for your family, as he continues in treatment. There is hope.
And to the media: there are many, many families like the Lloyds whose stories are newsworthy. Please don’t relegate schizophrenia to the back page until there is a celebrity affected - or, worse, an act of violence where untreated illness is suspected.
Our loved ones are worth fighting for.
Incarcerated Innocence: The Long Long Wait of Pretrial Detention
Seven months and counting, in pretrial detention. And no clear end in sight yet. This is a crime of the very system designed to rehabilitate, not just punish.
We need more beds for those with mental illness challenges, and we need them now. I know my son does.
Seven months ago, my son was arrested for “attempted purse-snatching”. He was identified as the “suspect” because the woman accusing him had video of him riding away on his bicycle. That’s it.
But what really incriminated him, I think, was his appearance. Ben has schizophrenia, managed currently by a medication with side effects of trembling and fatigue. Add to that the fact that he looked homeless at the time, and (truth) was probably stoned. After months of trying in vain to get a job, he had returned to his old addiction to marijuana.
So - the police had to decide - who to believe? The lady with the Louis Vuitton purse (still in her possession) or the homeless-looking young man with the confused, vacant stare?
Yep. Incriminated by his illness. It’s an old story, sadly.
What has followed, though, is another kind of crime.
My son’s bail was set at - get this - $100,000.
100K!
I’ve heard of murder suspects with lower amounts. Eventually it was reduced to 25K, but still. To be honest, I’d thought a week in jail, waiting for the court date, might not be a bad thing for Ben. He’d sober up, learn a lesson, get some structure back.
But that was nearly seven months ago. Still no evidence, and all sides have thankfully agreed (dozens of character references and court appearances later), that Ben qualifies for a jail diversion program that will give him treatment he sorely needs - substance use, mental health.
This is wonderful news, sure.
But there are NO BEDS. He is currently #10 on a waiting list at last report (haven’t had any response to further inquiries in weeks), and we can’t get updates. If only he could count down to a release date, so he’d know how long he’ll stay in jail, waiting for the chance to see the sunlight again.
Could be months, they said.
So Ben sits, with 55 other pretrial inmates, counting the days. Trying to stay positive, make some friends, help out the newbies. There are positives to knowing he is safe, sober, in a low-security situation more like a big room of “cube-mates” than a prison with bars. Thankfully, he has companions, a tablet, regular injections of his medication, and commissary access once a week. For this, I am grateful. Certainly, it could be worse.
But it is still, well, jail. Very little outdoor time, very little to do. Frequent lockdowns. One day just like the other. There are no self-development services for pretrial incarceration. No classes, no meetings, no opportunities to do anything except play cards, try out “prison cooking” and hope for mail or visitors.
Seven months. So far. And what breaks my heart is that I can feel the hope draining out of Ben. There’s only so much a mother can do - except love him, encourage him, listen to him, and advocate for a better system.
Ben is clearly one of hundreds, thousands, of incarcerated individuals who need treatment. And while he is one of the lucky ones who has been approved to get help, he sits there, still, in jail.
This is a crime. A crime of the very system designed to rehabilitate, not just punish.
We need more beds for those with mental illness challenges, and we need them now. I know my son does.
What’s a mother/conservator to do? I wrote to the public defender, the intake teams at the jail diversion program, the forensic social worker, the jail counselor.
Still no answers. Should Senators and Reps be next? I think so.
Don’t let him lose hope. And he is not the only one. We need change, and we need it now.
An Inmate's Mom: More Powerless Than Ever
You thought you had no say in your loved one’s care before? Try having a child in jail, awaiting a court date. He wears a standard uniform. You, parent and conservator, are also lumped into a category: inconsequential. You have zero power. No one returns your calls.
Well, here’s a new brick to add to the wall separating me from parents of “normal” children. I am now the mother of an inmate.
Ben has been arrested, and is in jail (not prison, I’ve learned the difference) awaiting his court date.
His crime? He’s accused of trying to snatch a purse (unsuccessfully, but it still counts as larceny). He swears he didn’t do it. It is the victim’s word against his. But my child - my man-child - looks like a thief these days. Though he has been living in a group home, he looks homeless. He won’t let a dentist fix his teeth. He has lost weight and his clothes are shabby because he wears them for days on end. Even his bicycle (which we just paid $500 to have repaired, good as new) looks homeless: the tire off the rim, the paint scuffed.
My son’s appearance itself is a liability when it comes to trust.
Did he do it? I hate to say this, but it is possible. Ben’s life, so filled pre-Covid with work and purpose (yes, even after diagnosis of schizophrenia, but on a different medication), has recently become scattered, desperate and empty. Covid had closed the restaurant business where he had worked for years as a popular server. That was when he lost everything that had given his life meaning.
Back in the hospital for nearly six months. Back on (different) meds after I’d called a hearing for a court order to medicate. Discharged to a group home.
Still. Ben had tried to make a life again. He had valiantly landed a retail job nearby. He’d d tried so hard to succeed at this. He’d walked 3.5 miles to get to work, always on time.
But his odd behaviors between injections of Haldol made him look distracted, even lazy. Of course he never disclosed his illness. He was eventually let go, and I think that’s what broke him. He lost hope after that loss.
Then: boredom, purposelessness, hopelessness. The perfect, awful storm for someone to turn to drugs for relief. What drugs? Can’t say, but we suspect more than marijuana, based on how quickly his money had been disappearing and poorly managed as of late.
Stupid schizophrenia.
The shock of his arrest has worn off for now, and as usual the best support is coming from those who have been there, the power of community. But there are now a lot of new things to learn - and the number one lesson is this:
You thought you had no say in your loved one’s care before? Try having a child in jail, awaiting a court date. He wears a standard uniform. You, parent and conservator, are also lumped into a category: inconsequential. You have zero power.
No one returns your calls. Not the public defender, not the jail “counselor”, not the Marshal's office. There is no way to find out if he is getting his meds, or where his backpack is. Your inmate child can call you, but you can’t call him. Can’t get a message to him. Can’t really help him, except to maybe pay for a lawyer other than the public defender.
So you learn, again, to let go of control, of influence - and even, a little bit, of hope.
The bar of what counts as the baseline of normal gets even lower.
Life with a child with schizophrenia. And now, clearly, addiction. And still worse now, one who has been arrested, fingerprinted, incarcerated.
Yet he is safe for now. And, oddly, doesn’t seem to hate it there in minimum security. He has more people to talk to, play cards and chess with, drink instant coffee with, than he has had in months. He has structure again. He has fewer choices - and is clean and sober.
The future? As always, I’m doing what I can, and letting go of what I must. The specificity of those choices is different now. The bar has indeed been lowered. But the stakes are higher than ever.
I hate schizophrenia - the great thief of lives that could have been. When will we fund research to find a cure, and improve the system that allows lives to get to this point?
The fight goes on.
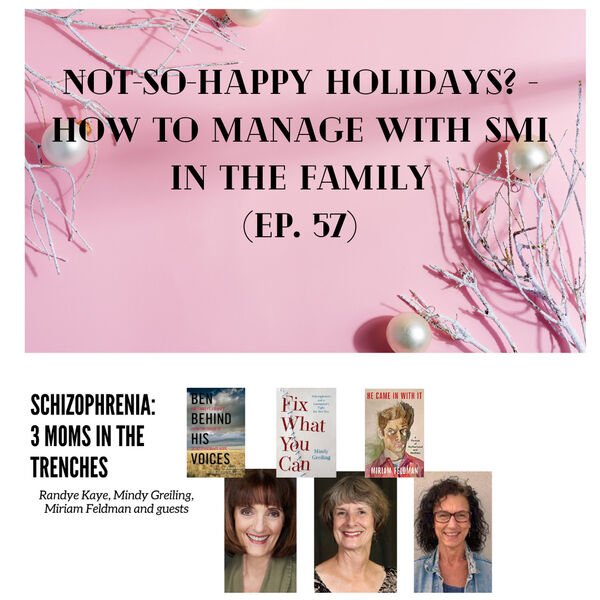
Not-So-Happy Holidays? How to Manage with SMI in the Family
What if, for families coping with SMI (serious mental illness) in a loved one, the holiday season is "the most difficult time of the year"?
The 3 Moms Discuss - Holidays past, in joy, crisis or grief - and how we currently celebrate what is...the best we can.
Some tips we share:
Lower Holiday expectations and Marketing Myths (e.g., perfect holidays)
Plan Ahead - even for possible disaster
Have a Plan B - and maybe C, D...
Include Your Loved One as Much as Possible, Especially if They Can Help
Don't Let the "Unsqueaky Wheels" feel ignored
Cherish the Good Moments - Find the Positives
Be Willing to Change Traditions as Needed
Set and Enforce Limits - Know Your Boundaries
Imagine How it Is for Your Loved One
Family Love Matters - You Do Make a Difference
Happy (and Realistic) Holidays to You All!
Want to Share Your Story in a Voice message?
Resources:
Look Again Podcast: https://www.bcss.org/lookagain/
Tips from NAMI: https://www.nami.org/Blogs/From-the-CEO/December-2021/The-Most-Difficult-Time-of-The-Year-Mental-Health-During-the-Holidays
Mindy and her book: https://mindygreiling.com/
Randye and her book: https://benbehindhisvoices.com/
Miriam and her book: https://www.miriam-feldman.com/
Growing Up Too Fast: When Your Parent has Serious Mental Illness
Our podcast, Schizophrenia: 3 Moms in the Trenches , continues - and to listeners who asked us, "what about the children raised by parents with SMI?" - we heard you.
This episode (42) is for you!
Guests: Karen Comba, author of The Snipers We Couldn't See: A Memoir of Growing Up with My Mother's Schizophrenia
And Christina Lord, mental health advocate (Canada) daughter of a dad with SZ,
First, your stories.
How has the experience impacted you (Karen writes about life “with footprints on her back”)
How did writing or sharing about it help? Or did it?
How did your experience- and the unpacking of it - inform the work you now do?
What do you most want other children of parents with SZ to know?
What do you want others to know - teachers, practitioners, other adults in a child-of’s life?
How to find happier places for your mind?
Links:
https://christinalord.ca/
https://www.karencomba.com/
Books we mention: (besides our own, Ben Behind His Voices, He Came In With It, and Fix what You Can)
She's Not Herself, by Linda Appleman Shapiro (formerly published as Four Rooms Upstairs)
I'm Not Alone: A Teen's Guide to Living with a Parent Who Has a Mental Illness, by Michelle D. Sherman
Happier Made Simple™: The 7 Core Phrases and Mental Illness in a Loved One
I cry, too - yet there is a way to be happier. The Seven Core Phrases (meant to be said to oneself, not as advice to others, please) and how they help me when our family deals with challenge or disappointment, especially regarding my son’s mental illness.
In the decade since Ben Behind His Voices was published, I've had the opportunity to tell our family story to a lot of people - sometimes more than once, for it is ever-evolving.
If you love someone with schizophrenia, you know this all too well. It is a life lived like a never-ending game of Chutes and Ladders, with moments of rest here and there.
The question I am most often asked, after sharing, is this:
"How do you stay so positive?"
Well.
When Life is Challenging…
It isn't always easy, as you may well know. But - here's the thing that continuously reveals itself to me, no matter what the challenge:
Yes, living happier is a function of what happens to you - no one gets through life unscathed, after all - but it is, eventually, even more a function of what you tell yourself about what happens to you.
And so, I finally wrote a book about it, and it launches officially in a couple of weeks.
In it, I talk about the "Seven Core Phrases" of self-talk that get me through most situations, and keep me hopeful, though realistic - and, yes, happier.
Yes, living happier is a function of what happens to you - but it is, eventually, even more a function of what you tell yourself about what happens to you.
It's how I "stay so positive."
Let me be clear (and I state it up front in the book) - I cry too.
Life isn't about constant happiness. That isn't even a goal. But neither is it about dwelling on the negative when the time for action has passed, nor about stressing about things that may never happen.
So here are the Seven Core Phrases (meant to be said to oneself, not as advice to others, please) and how they help me when our family deals with challenge or disappointment:
These phrases can set your mind down a different path of association and action. In case of severe trauma, you need to process the shock and emotions first.
Be Here Now: I use this when my son is in a good place (enjoy this conversation; savor the moment; enjoy his company) - and when he is not (this is where we are right now - what action do I need to take?)
It Is What It Is: This gets me past the moments of regret (why didn't I see the signs earlier?). disappointment (why was my son robbed of a chance to go to college?), and doubt (why me? why him? why us?). There may be no reason for Ben's illness. It simply is. Now what?
We're All Connected: Other families are going through this too. Other people have the illness. Let's talk about it. Let's help each other. Let's reach out. Let's thank the people who have chosen professions that help us (lawyers, social workers, advocates, psychiatrists, etc.)
This Is Good: Savor the moments when the stars align, and your loved one can communicate, eat dinner with the family, etc. Yes, even during Ben's ten hospitalizations, when the phrase simply meant "enjoy the vacation from caregiving for now." We remember what we savor, and learn from what we regret.
All Will Be Well: Depends on how you define "well." Will Ben ever attain his childhood dreams? Doubtful, at least right now. We learn to adjust our dreams. And I have no idea if the Universe has a "Plan" - but sometimes it helps to believe that it does. Whatever gets you through. As I say in my book: All will be well, just maybe not the way your expected it to be.
Isn't That Interesting?: Curiosity, and even humor, can lurk underneath the trauma and crises. There have been times (especially when in the company of others who get it) where humor has saved me from crashing; when curiosity instead of complaining led me to learn more, do more, find another way.
Whatever Happens, I'll Handle It Somehow: This gets me through more times than I could ever list. Loving someone with schizophrenia means a lot of second-guessing, a lot of waiting to see if the meds work, if they'll come home, if they will be Jekyll or Hyde at the family dinner. So we do what we can to prepare, and hope for the best after that. This phrase gets me through the times where worry is unproductive.
Want the book? You'll find it now on Amazon, in paperback or kindle - but pssst! On launch day Feb 23 the kindle will be only 99 cents for a limited time! - and I am now working on the audiobook.
I hope it helps. Even a little.
Randye
After Mental Health Treatment - What? Fellowship Place Gets it Right
This community is called Fellowship Place, and it represents what can happen when people come together to look past medical treatment alone - and add housing, purpose, structure, and community to the picture.
Ten years ago, I toured a community with the following mission:
To serve adults living with mental illness by offering a full range of therapeutic support and rehabilitation services that promote independence, wellness, and a meaningful life.
This community is called Fellowship Place, and it represents what can happen when people come together to look past medical treatment alone - and add housing, purpose, structure, and community to the picture.
At the time, I wished Ben might be interested in living in such a caring, well-thought-out community. He wasn't. But now, ten years later, he is open to the idea.
The only problem is: it could take a decade before a place opens up. I wish I'd put him on the waiting list ten years ago. It might take that much time.
We need more places like this.
Hear why:
Channeling Grief and Anger into Advocacy and Acceptance
Mimi Feldman, Mindy Greiling and I have been co-hosting our podcast, Schizophrenia: Three Moms in the Trenches, for almost a year now. Our 32nd episode this week has garnered more YouTube viewings in its first two days than any other so far, and guest Jerri Clark, our " Fourth Mom in the Trenches" for this episode, is the reason.
If you want to know more, please subscribe to the podcast on itunes or wherever you get your podcasts, and/or on YouTube. Our facebook page is @schizophrenia3moms.
Here are some of the notes:
What if: the mental health system would pay more attention, take more steps to help , before tragedy, violence, or crime finally calls attention to symptoms of SMI (serious mental illness)?
What if Darrell Brooks (charged with murder after plowing his mother’s car into a parade in Wisconsin) had been helped, and treated, instead of ignored or imprisoned? His mother, Dawn Woods, wrote a letter to the media. She, too, is a “mom in the trenches”. So is journalist/advocate/mindfulness coach Jerri Clark, our guest for this episode.
What if Jerri’s son Calvin had received treatment, despite his “civil right ”to refuse it - although the refusal itself is a symptom of his illness?
She says:
Difficult: Mothering Challenging Adult Children through Conflict and Change, Book Review
Author Judith R. Smith had me at the first glance of the callout quotes:
"You can divorce a difficult spouse. It's much harder to give up on a difficult child."
and
"When a child is diagnosed with serious mental illness, they do not die - but they are changed."
How do we continue mothering, when our children are long past the age when we thought we'd be graduating from the phase of hands-on support? What do we do, what do we feel, what do we fear when our stepping aside could spark poverty, homelessness, even violence for our children?
In this thorough, empathetic account of this important previously-swept-aside issue, Judith R. Smith combines eight years of research and grimly honest stories from mothers of children who have SMI (serious mental illness), addiction, and other issues we never expected to face in our kids.
We learn about the problems presented by not only our own family challenges, but also cultural expectations about motherhood and system failures of support. We feel less alone when hearing the stories and reading the facts. Then, Smith takes us through steps including attitude change, getting support, practicing self-care, and ways to stay safe and possibly even help our grown, difficult, children.
There has never been a book like this. If you're a mother still inside the journey no one wants to speak about, get this book. You'll be glad you did.
Available February 2022, Rowman and Littlefield
Schizophrenia: Nearly Everyone is a “Long-Hauler”
We Need a Cure
The scariest thing about Covid-19, once you’ve been lucky enough to survive it, is a set of residual symptoms that are still being discovered. I’ve heard everything from “it’s a year later and I still can’t taste my food” to “I still get winded six months later and can barely walk up a flight of stairs” to stories of teeth suddenly and mysteriously falling out months after recovery.
People experiencing symptoms like these are called Covid long-haulers. There are Facebook pages and groups where stories and support are available.
But my son, Ben, and others like him? Schizophrenia long-haulers. This is the brain illness that just keeps on “giving” - challenges, changes, symptoms, side effects, loss.
This illness never quits. The residual symptoms sure do beat the active symptoms like psychosis and crisis, but they are still hard to bear.
Everyone is a long-hauler with this brain disease.
We need a cure.
My son is doing okay - actually better than expected - on Haldol now. This older antipsychotic frightens me, because side effects like tardive dyskinesia can be irreversible. Also, it is not known to work on the “negative” symptoms of schizophrenia (things the illness takes away from the person, like ability to feel joy). Still -it’s not too bad.
Some good news: (must mention, Ben no longer lives with us, so some of this may be due to the excellent staff at his group home, and a life less dependent upon our family role as landlords etc)
I can converse with him. Actual give-and-take conversation.
We have actually watched an entire movie together.
He eats my cooking again, after years of saying “smells great, I’ll have some tomorrow” (I think he had some sort of belief about my food that prevented him from ever taking a bite in those years).
He has also gone swimming again, and plays beautifully with his nieces and nephews. In fact, they have a relationship with “Uncle Ben” for the first time in years.
Haldol is available as an LAI (long-acting injectable) , so Ben isn’t faced with a daily decision as to whether he “needs” antipsychotic meds or not.
But, some of the sadder news:
I do see some trembling in his hands now. Would he ever be able to work as a waiter again, the job that kept him afloat before Covid closed restaurants?
He is suspicious of doctors, dentists and any medical testing. This is fairly new. He will not have his teeth cleaned.
When he isn’t hyper- focused on something I see the eyes darting around the room again, and wonder what he hears and/or sees. He will NOT talk about this, or admit to it.
He talks once again about unrealistic plans - like opening his own restaurant, becoming a college professor.
This illness never quits. The residual symptoms sure do beat the active symptoms like psychosis and crisis, but they are still hard to bear.
Everyone is a long-hauler with this brain disease.
We need a cure.
Daring to Hope Again: Faith or Foolishness?
The game of Schizophrenia Recovery Chutes and Ladders (or Snakes and Ladders, for you Brits) continues.
In the past few weeks, Ben has climbed some ladders, made some progress. Yesterday's family visit was full of simple pleasures again:
a car ride that was full of conversation, not the torture of awkward silence and small talk
Ben and a friends watched a movie in our living room and actually made it through the whole thing
We talked about his future, his feelings, his sobriety journey (now counting again, 15 days)
Ben was less defensive, more forthcoming
I brought up my concerns about his current med (Haldol) and my wish that someday he might try Clozaril again so as to avoid the side effects (tardive dyskinesia, mainly) of the Haldol - and Ben seemed to listen. (not agree, but he did listen)
These days are miracles. These days give me hope, though I've learned not to predict beyond a good day.I don't predict. But I can hope.
I can hope that Ben will continue to value his sobriety and the meetings that help him.
I can hope that the side effects of the Haldol are not permanent.
I can hope that he can again be a part of family celebrations.
I can hope that, perhaps, one day, he will gain insight into his illness and serve as an inspiration to others.
I can hope that he will, again, be able to work, to have friends, to feel purpose and joy.
I can hope for a cure for schizophrenia.
Hope is not foolishness. Hope is a celebration.
If I'm wrong, at least I'll have had a day of seeing my son's smile again, or actually enjoying talking with him, of seeing that he might be able to get some of his life back.
And that I can't do it for him. All I can do is love him (always), set limits (whenever I have to), and do the behind-the-scenes advocacy that is necessary to keep him afloat.
(where are his social security benefits? Does he have money to pay his rent? Can he work again someday? Where? How? Are there activities he can participate in right now, to give him the structure and purpose he lost when he lost his job due to Covid and then turned to smoking weed instead? ....the list goes on. We orchestrate behind the scenes.)
A good day. I'll take it.
"Mom, My Future Seems So Bleak": Feeling the Heartbreak
My son. He is trying to hard to get his life back. If he weren't trying so hard, maybe then I could detach - let go just a little bit more than I've already trained myself to do.
But it's heartbreaking. For me, sure - but mostly for him.
The trouble with regaining some sanity (or sobriety, for addicts) is that your vision, when examining your life, clears. That, unfortunately, can hurt like hell.
I can feel why, sometimes, it may feel easier to just fall down the rabbit hole of non-treatment and go back to a problem that's more familiar: getting out of the hospital.
Square One (or two, or three), when you've climbed so far ahead of it in the past, is really a hard spot to land back on. Ouch.
The trouble with regaining some sanity (or sobriety, for addicts) is that your vision, when examining your life, clears. That, unfortunately, can hurt like hell.
That's part of why a fresh obstacle to Ben's renewed recovery journey (after the Covid-19 fall) is now: getting clean. He has returned to smoking pot - never a good sign - which brings all the usual "side effects": lies, denial, the illusion of accomplishment, poor decisions, loss of money, lack of motivation.
Shit.
Road to recovery…Far from Clear
The first signs were during a home visit - halfway through a fantastic visit, after Ben "took a walk to Starbucks", he returned home completely stoned. And denying it. I took him back home and told him he could lose his placement in the group home, and also I would not be allowing him to visit until the truth - and a plan of action - came through.
One day later, a very contrite Ben called to apologize, in tears, and ready to tell the truth and "get clean"...and he did - for 35 whole days. He even went to meetings, and shared for the first time ever. Yeah, maybe "it's only pot", but for Ben it spells disaster.
Then...a relapse. He took 2 hits from "some girl on the street corner" (after refusing once, but then he caved) because "I thought it wouldn't really make me seem stoned, and it might make me feel better about my life."
Another call from his Group Home.
Another frantic message of denial from Ben
He can lose his housing. He lost his home visit. I feel stuck in a cycle of Groundhog Day-like repetition.
I gave Ben a day to come clean with the truth - and he did. We talked for over an hour. He is so angry with himself. He regrets giving in to temptation. He says all the right things...but he has said them before.
Still - what breaks me apart are two things: his voice, cracking with tears and emotion (rare for those suffering with schizophrenia), and his statement:"
Mom, My future just feels so bleak."
Oh. My.
He has lost everything he works for years to build - his work, his car, his friends, his sanity, his place in our home -- and months of his life. Unemployment is a huge blow - I've been there, and so has my husband, and maybe so have you - but imagine going through it when you've also "woken up" from the longest hospital stay of your life, to find that your world has fallen apart.
And now - some steps we've all agreed to, to provide more purpose and structure. Yes, he wants to work again someday - that waiter job was everything to him (but can he work? with hands trembling from Haldol? we shall see) - but for now, all I can do is remind him that:
he has rebuilt his life before, and can do it again
there are people who want to help
Getting too cocky, and thinking you can get sober alone, seldom works for him - and is often a sign of danger.
We love him
For now, it is good to sign up for some activities offered to him, even if they fall short of the full-time work he used to have.
Here's where we are. Ben is in a group home. He is rebuilding again after a 5 1/2 month hospitalization.
The Four Pillars, our present day version in this new Recovery Journey:
Treatment: Haldol by injection (different medication for Ben than the one he'd done so well on - in my eyes - before, but he swears he "likes it better".
Plus Side: Injection form much easier to manage (time-release)
Minus side: I am seeing tremors (could become permanent). Ben hides these, and denies their existence.
Structure: Some. Group Home meetings, and now some "Anonymous" meetings. He needs much more structure. Don't we all. He fills his time taking long walks, but his life is too aimless (considering pre-Covid he worked full-time)
Purpose: He was stripped of it when Covid cost him his job. Purposelessness sucks.
Community/Love: Well, he still has us, his family. But now it's weekend visits, and only if he is clean and sober. He has lost the right to visit us more than once - along with my trust.
So - we move ahead. With new steps. One day at a time.
2 days clean/sober, and he has also learned some things. Hopefully they will stick.
Hope for "Normal" Days Springs Eternal
"Mom, I sometimes I thought I'd never actually have a pleasant day with Ben again. Today was so great!"
Exactly my sentiments, honey.
Families of those with Schizophrenia know: "normal" days are miraculous. And we treasure. Every. Single. One. Because, well, we might not get more of the same. no guarantees.
Hope springs…and sustains
Blog followers here know that we've had quite a few, um, adjustments to make re Ben in 2020-21. From full-time employment to hospitalization, to back in group home care...and now, addiction to contend with. It has been a tough year for us, sure --- but so much worse for Ben, especially now that he is "well" enough to realize that his life has gotten so messed up.
He has lost so much.
Stupid Schizophrenia. Thief of lives. Robber of relationship. Obstacle to useful employment. And so much more.
And yet. There is hope - and moments to treasure again. Grateful, grateful for:
Ben, 25 days clean now. (his addiction is marijuana). One day at a time. He is going to meetings. Fingers crossed. But - wow - it is so different when he isn't stoned.
Two days in a row of family fun - yes, fun! Ben is on Haldol now - not my favorite, as I fear the permanent side effects, but Ben seems happier on it. Letting go of control...as best I can. It's his life. But I must say that things are better than expected, even though Haldol doesn't do much for the "negative symptoms" of his brain illness.
But - some miracles in the past few days, on family visits:
He went swimming! He used to love it so much as a boy, but for some reason hasn't gone in the pool for five years (I suspect some sort of psychosis belief that kept him away, but I'll never know for sure) -it was always, "Maybe next tiem" - but he went swimming with his young nieces and nephew, and actually played with them. Played!
We did a family trip to the local Aquarium and Ben was actually helpful - the kids adore him, and he was present and involved. And - during lunch, he turned to his sister (as the kids were doing their "I-haven't-been-to-a-restaurant-since-Covid- and-forgot-how to-behave" routine) and said, "wow, sis, you have your hands full, don't you?"
Empathy!
If you have a relative with SZ, you know what a miracle this is.
Yeah, he's trembling a bit, and I fear the presence of tardive dyskinesia - a possibly permanent side effect of the med Ben is on.
But all we have is today, and what is, is.
So I'll take the miracle of having made some more good memories with my son. Grateful And always hopeful, and ever watchful.